Analyzing S100A8 expression can indicate early evolution of melanoma in the surrounding cells of the skin tumor microenvironment
By BRANDON NGUYEN — science@theaggie.org
According to the National Cancer Institute, melanomas, a type of skin cancer that occurs in cells that produce melanin, are the fifth most common cancer type in the United States and cause the vast majority of skin cancer-related deaths. UC Davis Health recently published a study that established reliable cellular biomarkers that point to early development of melanoma.
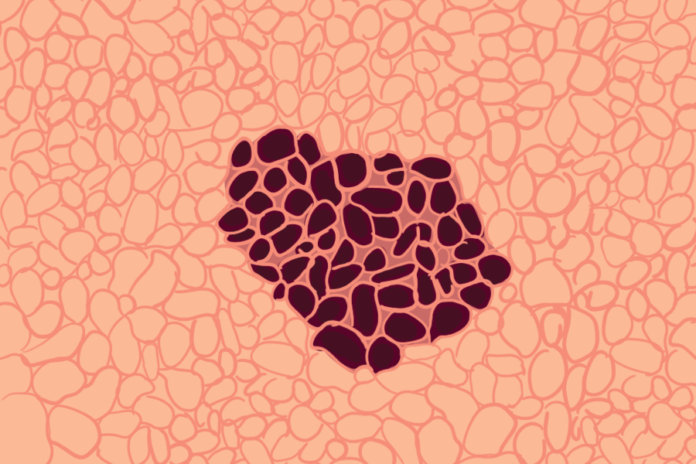
Within the top layer of skin, there are different skin cell types, including melanocytes that produce melanin skin pigments and keratinocytes that produce the protein keratin, which is important for skin durability and hair strength. The study published in the Journal of Investigative Dermatology notes that “[e]arly diagnosis of melanoma is critical for improved survival. However, the biomarkers of early melanoma evolution and their origin within the tumor and its microenvironment, including the keratinocytes, are poorly defined.”
Melanomas arise from a multi-step process in which melanocytes mutate and proliferate uncontrollably, in effect producing a tumor of skin cells. Curing this cancer involves properly diagnosing and treating it early in its development.
Dr. Maija Kiuru, a practicing dermatologist and dermatopathologist at UC Davis Health and the lead author on the study, explained how melanomas are typically detected and treated.
“Melanomas are typically found on skin exams, either by a physician or by the patient or a family member,” Kiuru said via email. “One screening tool is the ABCDEs of melanoma (a lesion with asymmetry, irregular borders, variable colors, large size, and evolution over time). Diagnosis is made by a skin biopsy and histological examination. Treatment for most melanomas include surgical removal, and in more advanced cases, the treatment will include lymph node sampling and systemic therapies.”
Dr. John McPherson, a professor in the Department of Biochemistry and Molecular Medicine at UC Davis Health and corresponding author on the study, elaborated on mutations that lead to melanomas.
“You have about 3 trillion cells in your body, and every day in every cell, there’s about 10,000 damages to your DNA, which are repaired,” McPherson said. “There are very amazing biological mechanisms that find and fix the damaged DNA, and if they can’t, then they usually program the cell to die. Mutations in these mechanisms can lead to cancers like melanomas, and about 40 to 50% of melanomas have a very specific mutation in a gene called BRAF with a very specific amino acid change in the 600th position.”
BRAF is a signaling molecule that takes signals from outside that come down a cascade and then tell the cell to grow and replicate, according to McPherson. Mutations in this signaling molecule — that acts as an accelerator for the cell— lead to uncontrolled growth or cancer.
The study that both Kiuru and McPherson collaborated on focused on identifying genes that can serve as markers for melanoma development and to improve diagnosis of melanomas.
“We all have moles and funny little things on our skin, and sometimes they might look like melanoma, and the idea is to identify what really is melanoma and what is not,” McPherson said. “So many things are cut off and then they’re biopsied, and even when they’re biopsied and analyzed under the microscope, pathologists sometimes aren’t sure. If you get a bunch of pathologists in a room and say, ‘is this melanoma?’ you might get varying opinions. What we really want to do is be able to clearly say ‘okay, this funny-looking thing that we’ve biopsied is definitely melanoma.’”
Both authors examined the expression of over 1,000 genes in 134 regions of interest enriched for melanocytes as well as neighboring keratinocytes or immune cells. The tissue examined came from patient biopsies from 12 tumors, ranging from benign to malignant.
“We utilized an approach that looked at gene expression of hundreds of genes directly on glass slides that contained melanomas and nevi ([also known as] moles, the benign counterpart of melanoma), without disrupting the architecture of the tumor,” Kiuru said. “This is called spatial gene expression profiling and [it] is helpful in better understanding the interplay between tumor cells and their neighboring cells, like immune cells and epithelial cells.”
According to McPherson, molecular tests for diagnosis and prognosis of melanomas are on the rise, but markers for early melanoma development remain lacking. This study serves as a stepping stone to shed light on potential biomarkers that allow for early treatment of melanomas and increases the odds of curing the cancer in patients.
“We found that melanoma biomarkers are expressed by specific cell types, some by the tumor cells but others by neighboring cells in the so-called tumor microenvironment,” Kiuru said. “The most striking observation was that S100A8, which is a known melanoma marker thought to be expressed by immune cells, was expressed by keratinocytes that make up the outermost layer of the skin called the epidermis. Melanoma biomarkers in the epidermis have been largely overlooked in the past.”
The study found that S100A8 expression was exclusively found in melanoma cells and not benign tumor cells, which make this biomarker a potentially good indicator of early melanoma. Kiuru said that this biomarker is one of many that shows how important having a cellular tool for early detection of a cancer is key to the overall survival of the patient.
“This study revealed new markers of melanoma and new roles for previously-identified markers that may facilitate a more accurate diagnosis of melanoma, leading to improved survival of patients with melanoma,” Kiuru said. “A similar approach can be taken with other cancer types.”
Written by: Brandon Nguyen — science@theaggie.org