Research could lead to cure of both type I, type II diabetes
An estimated 29 million Americans live with diabetes and 86 million live at risk of the disease, which is recognized as a nationwide epidemic. However, the recent discovery of a new type of pancreatic cell may serve as an alternative insulin source to help those diagnosed with type I and type II diabetes.
The discovery of this new cell was published in Cell Metabolism by Mark Huising, a UC Davis assistant professor of neurobiology, physiology and behavior.
“Looking at how common diabetes is, this is not isolated to scientific discovery,” Huising said. “It impacts us all, and we have or know somebody with this health problem.”
Pancreatic cells, specifically beta cells, produce insulin to control the amount of glucose, also known as sugar, in the blood. People with diabetes do not make enough insulin (type I), or cannot use insulin properly (type II).
High amounts of blood sugar can lead to health effects such as heart disease, kidney failure, stroke, blindness and lower limb amputations.
Huising and colleagues unveiled a new type of insulin-producing cell that could lead to replacing nonfunctional or depleted beta cells in the pancreas.
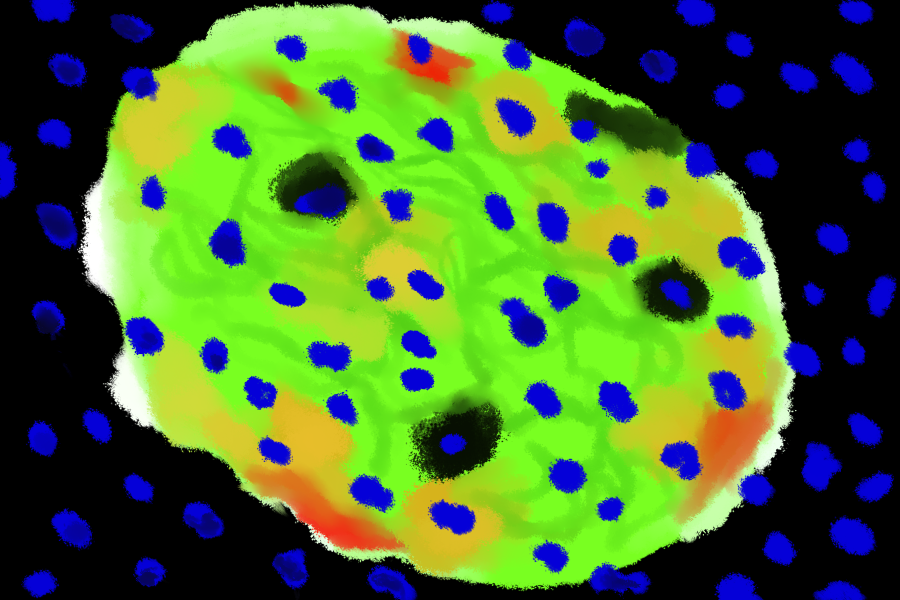
Through the use of specialized microscope imaging, scientists located a new type of cell around the pancreatic edges of islets. The observed cell had similar appearance to an immature beta cell.
Scientists concluded that these new cells are able to produce insulin, but they do not have the receptors to detect glucose, and are therefore unable to function as a full beta cell. These immature beta cells are actually at an intermediate stage, between the mature beta cell and the mature alpha cell, also involved in blood sugar regulation.
This study is the first time that critical cells in the adult stage can transform into a highly needed cell, such as the beta cell.
“This transformation is happening all the time in normal healthy islets, and occurs even in the absence of disease or injury,” Huising said.
Plasticity, or the ability to change, is a widely researched topic, but not in a manner similar to Huising’s. This research identified plasticity in a different angle, looking at it in minority cells, or cells that are not fully mature. Minority cells transdifferentiate, or naturally change from one cell into a different cell type.
This new beta cell population is unique because the nature of it has never been characterized before or identified in adults.
This research was accomplished through new order image strategy approaches. The new cell was identified via labeling in imaging. Traditionally, researchers kill the cell or tissue being examined and then induce staining to see it more clearly under magnification.
However, the novel discovery of immature beta cells was observed during live staining methods.
“Using confocal microscopy, we are able to image the cells alive,” said Dr. Siming Liu, a researcher at Huising Lab. “That is the unique part of this data included in the publication.”
An incorporated fluorescence protein was added so that scientists could label specific cell type. In this method, the stained tissue can be isolated and it is still alive.
The immature beta cell was observed in both mice and human tissue, prompting the idea that these cells could be conserved in other species as well, although it has not been confirmed.
Analyzing and organizing the genetic data collected can be accomplished in multiple ways. Regarding the context of Huising and colleagues’ particular questions, the interest mostly lied in identifying the genetic components that underlie the behavior of the immature beta cell.
“I used a computational approach to explore the differences between immature and fully mature beta cells, as well as the alpha transdifferentiate cells,” said Alexander Mawla, an author of the study and a UC Davis integrative genetics and genomics graduate student.
Not only does this this new population have the potential to serve as a replenishing source of the affected beta cells in type I diabetes, but they can also help understand the condition of cells with those of type II diabetes.
“The field used to think that beta cells in type II diabetes die, but more recent insight suggests that they regress into a state that is no longer functional,” Huising said. “And because these cells are still around, it gives us an opportunity to see if we can coax these cells back into functional cells.”
The immature beta cells may also help to develop stem cell therapies, since stem cells are undifferentiated and capable of developing into a wide range of other cells.
“[The immature beta cell population] gives us a blueprint on how we can make functional beta cells from stem cells,” Huising said.
Currently, growing real beta cells from stem cells has proven difficult because they are missing some traits and the full functionality that standard beta cell have.
Although much information is provided to the public with regard to managing and preventing diabetes, such as the CDC website, its widespread prevalence is cause for further research. In order to advance human health, it is essential researchers publish and share their findings.
“People reading this [publication] can understand how the biology performed in labs can be applied to health issues such as diabetes,” Liu said. “[As well as] applying their scientific knowledge to help studying this disease, and others as well.”
Written by: Shivani Kamal — science@theaggie.org



