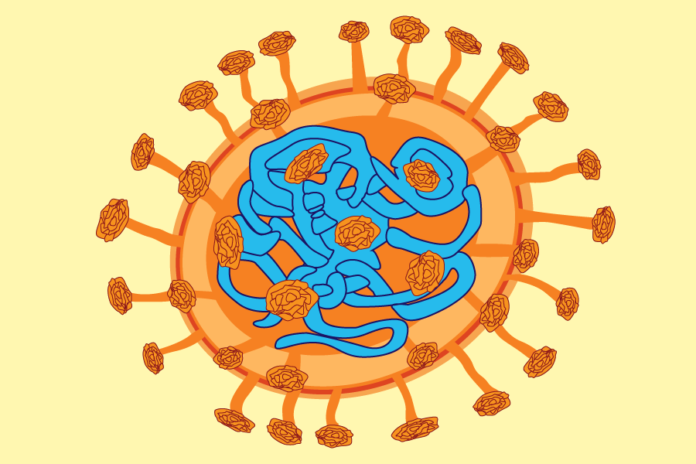
The Delta variant has more efficient transmissibility with selectively advantageous mutations in its spike protein
With recent anticipation and plans for students to return to campus this coming fall, the Delta variant of the coronavirus has brought yet another wave of cases that continue to plague the population of both the vaccinated and unvaccinated alike.
“For most of June, there were fewer than 10 patients with active COVID-19 at the UC Davis Medical Center on any given day,” according to a recent UC Davis Health press release. “On several days there were five or six. This week, it’s ranged from 18-25 patients daily. And UC Davis Health experts expect that to go up.”
Dr. Brad Pollock, the chairman of the Department of Public Health Sciences at the UC Davis School of Medicine and a distinguished professor trained in epidemiology, describes how variants like the Delta variant arise from the original coronavirus.
“Like many other viruses, there are opportunities for the virus to sort of get better at what it does, that is, to mutate,” Pollock said. “So with large numbers of people infected and lots of viral replication going on all the time, there can sometimes be what we would call errors. Random mutations that occur in the genome for the virus can confer a selective advantage. The major changes that have occurred with these variants, and these are sometimes called variants of concern, is that the virus has gotten to be more infectious. Another one is that the virus could theoretically become what we call more virulent or create more disease.”
The Delta variant is just one of many mutations that the original coronavirus has undergone but has become stably effective and potentially more dangerous. Though this variant has not caused any patient to feel sicker, it has become far more contagious.
“This virus is thought to be about 60% more contagious than the original wild type strain,” Pollock said. “That means that it’s just that much more likely that if you’re in some proximity to somebody who is infected and you’re not protected yourself, you’re more likely going to acquire the infection.”
Fortunately, those who were vaccinated but still ended up falling ill to the variant have not required hospitalization and have experienced a milder version of symptoms of the coronavirus.
Dr. Christian Sandrock, a critical care doctor at the UC Davis Medical Center working with patients infected with the coronavirus, further explains the dangers behind the Delta variant.
“The Delta variant isn’t necessarily more deadly,” Sandrock said. “It’s definitely more contagious, and it spreads more rapidly, particularly in non-vaccinated communities. This variant just has some features associated with the spike protein and some of the other proteins that help enhance transmissibility and also better evade our immune system. What we have seen–again, it’s anecdotal–is that certainly the age group between about 30 and 50 seems to be hit a little bit harder.”
According to the recent UC Davis Health press release, Sacramento County has the third highest COVID-19 case rate in the state, with 11.5 cases per 100,000 people over the last seven days. The county’s vaccination rate is around 50%, well below the statewide rate of 63%.
While both Pollock and Sandrock agree that the variant, which accounts for the rise in the majority of cases currently, will not lead to another quarantine period, they both warn that a return to normalcy requires getting the unvaccinated population vaccinated as soon as possible.
“You probably heard that Pfizer was working on trying to get FDA approval for a booster, and the federal authorities FDA and the CDC are saying, well right now, that’s not the real problem,” Pollock said. “And they’re right, because the real problem right now is that we have 40 to 50% unvaccinated. It has nothing to do with the booster shots. This has to do with folks that are not protected at all who can harbor the virus, and the more people who get infected, the more likely that there is to be a mutation that arises that is even more favorable than the Delta variant.”
To avoid future outbreaks like the coronavirus, Sandrock, in the same vein as Pollock’s view of prioritizing the urgent need for vaccinations, provides insight into the need to improve our public health system.
“To really survive a larger pandemic or a deadly outbreak, there has to be strong public health infrastructure and societal cooperation to that public health infrastructure,” Sandrock said. “So not only does there need to be society’s investment in public health but also society’s trust back into the public health community. And we do not have any of that right now, which is the most surprising part of the pandemic right now. So the one lesson is that this needs to reverse itself or the next pandemic is going to be exceedingly more deadly.”
Written by: Brandon Nguyen – science@theaggie.org