Cytokines TNF and IL-6 can cause severely damaging inflammatory effects as a result of stem cells attacking host cells of blood cancer patients
By BRANDON NGUYEN — science@theaggie.org
Researchers at the UC Davis Medical Center recently discovered a novel treatment against graft-versus-host disease (GVHD), a potentially lethal inflammatory condition that can arise following stem cell transplantation, which treats blood cancers and disorders. Allogeneic Hematopoietic Stem Cell Transplantation (allo-HSCT) to treat some blood cancers and disorders involves injecting a donor’s bone marrow stem cells, also known as graft, into blood cancer patients undergoing chemotherapy and radiation therapy.
Dr. William Murphy, a professor at the UC Davis School of Medicine under the Department of Dermatology and Internal Medicine and senior author of the study, further explained what GVHD is under the context of blood cancers.
“If we take stem cells from another source, usually trying to match as much as we can from a related source such as a sibling, there seems to be an anti-tumor effect,” Murphy said. “This desired, beneficial effect from stem cell transplantation is called the graft-versus-tumor (GVT) effect. But the graft-versus-host disease means those immune cells can also attack not just the cancer, but the recipient or patient, which occurs pretty often.”
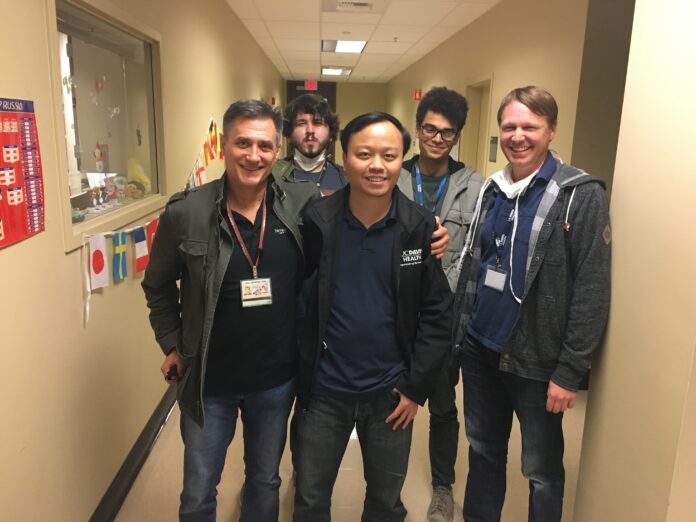
The medical dilemma Murphy and his team of researchers faced involved maximizing GVT effects while minimizing GVHD during stem cell treatment to help the patient effectively fight off the tumor. Logan Vick, a graduate student under Murphy’s lab at the UC Davis Medical Center and a co-author of the study, talked about the major findings that help minimize GVHD in allo-HSCT patients.
“In graft-versus-host disease, something that can be picked up as a symptom is this release of cytokines, which are inflammatory proteins,” Vick said. “TNF and IL-6, which are two inflammatory cytokines, are often used as tools of the immune system to combat either viruses or different pathogens, but prolonged inflammation can have consequences. So by blocking these two cytokines, what we call a dual cytokine blockade, can help ameliorate GVHD.”
The cytokines, TNF and IL-6, that Vick focuses on can cause a “cytokine storm,” which can occur during GVHD when donor immune stem cells attack the host’s healthy cells instead of the tumor and induce inflammation caused by cytokines. GVHD and the dangerous “cytokine storm” effect has been a problem for stem cell transplantation treatments, but Murphy’s team of researchers have just found a potential cure to GVHD while still maintaining the efficacy of the treatment.
Lam T. Khuat, a postdoctoral researcher at Murphy’s lab and the first author of the study, summarized the beneficial results from dual cytokine blockage.
“Many treatments for GVHD involve suppressing the body’s immunity, which can inhibit beneficial GVT effects,” Khuat said via email. “For this reason, it was important to determine if blocking these cytokines impacted the GVT response. Fortunately, anti-tumor effects remained after the transplant and with the combined intervention.”
Clinical methods have often employed single cytokine blockades; however, with the novel finding that dual cytokine blockades can minimize the proinflammatory responses induced by GVHD, the treatment can also be applied in other health conditions that require stem cell transplantation or reducing inflammatory side effects.
“Normally, when you have an overactive immune system, whether it’s autoimmune disorders or GVHD or even in viral infections, the treatments sometimes blanket immunosuppression with steroids,” Murphy said. “Well, that works because they turn off the immune system, but in the case of cancer and viral infections, you want a working immune system. The beauty of using this double block, which can be applied in other clinical settings, is it doesn’t suppress the immune system while preventing the inflammation and the damage.”
Written by: Brandon Nguyen — science@theaggie.org