A combination of surgical Targeted Muscle Reinnervation and machine learning helps patients make more complex upper limb prosthetic movements
By BRANDON NGUYEN — science@theaggie.org
A team of UC Davis scientists and reconstructive surgeons is collaborating to improve the quality of life for patients with upper limb amputations. Through a novel surgical procedure called Targeted Muscle Reinnervation, surgeons can rewire residual nerves surrounding a patient’s amputations to reduce nerve ending pains.
Dr. Clifford Pereira, an associate professor in the Plastic Surgery Division at the UC Davis Medical Center, described the pains that patients with amputations typically accumulate.
“When amputations are done, the main nerves going into the muscles in the part that has been amputated, those nerves are traditionally either dumped into bone or muscle,” Pereira said. “If you leave the nerves where they are, they try to regenerate and find a partner on the other side. And because the other end is not available to connect, they end up forming these live fibers that are right under the skin that can be very painful.”
Nerve ending pains, or neuromas, are just one of the two main pains that can develop into large lumps, according to Pereira.
“The second thing is the same nerves give the sensation to the brain that the missing hand or foot is still present,” Pereira said. “This is called a phantom pain, so people still feel pain in the foot, although the foot is not present anymore, and they also feel like they’re still attached to the foot.”
Targeted Muscle Reinnervation is a surgical procedure that reroutes these nerve endings to a nearby muscle to reduce these two primary types of pain, which can become unbearable. As a result, patients often undergo prosthesis abandonment, leading to a reversion back to the old hook and cable system that does not require the use of a smart device.
“I recently worked on this patient that had an arm amputation, and when I went into the operating room, he had four neuromas that were almost the size of golf balls,” Pereira said. “He was on chronic pain medication for the last four or five years with very high doses of opioids. As soon as we did the surgery [Targeted Muscle Reinnervation], he no longer needed the medication, no longer felt any discomfort, and it changed his life.”
Dr. Andrew Li, another reconstructionist surgeon working alongside Pereira at the UC Davis Medical Center, explained how this surgical procedure is crucial not only for resolving pains from amputations but also for improving the patient’s quality of life.
“It has become increasingly apparent that restoring the muscles to their normal physiology has benefits not only for prosthetic control, but also for a patient’s day-to-day mental well-being,” Li said.
In addition to surgical reassignment of nerves, surgeons are working with mechanical engineers and neurologists to improve patient control of complex upper limb prostheses movements.
Dr. Jonathon Schofield, an assistant professor at UC Davis’ Department of Mechanical and Aerospace Engineering, is working with Dr. Wilsaan Joiner, a UC Davis neurologist, to optimize smart prosthetic devices to better predict the movements of patients with upper limb amputations.
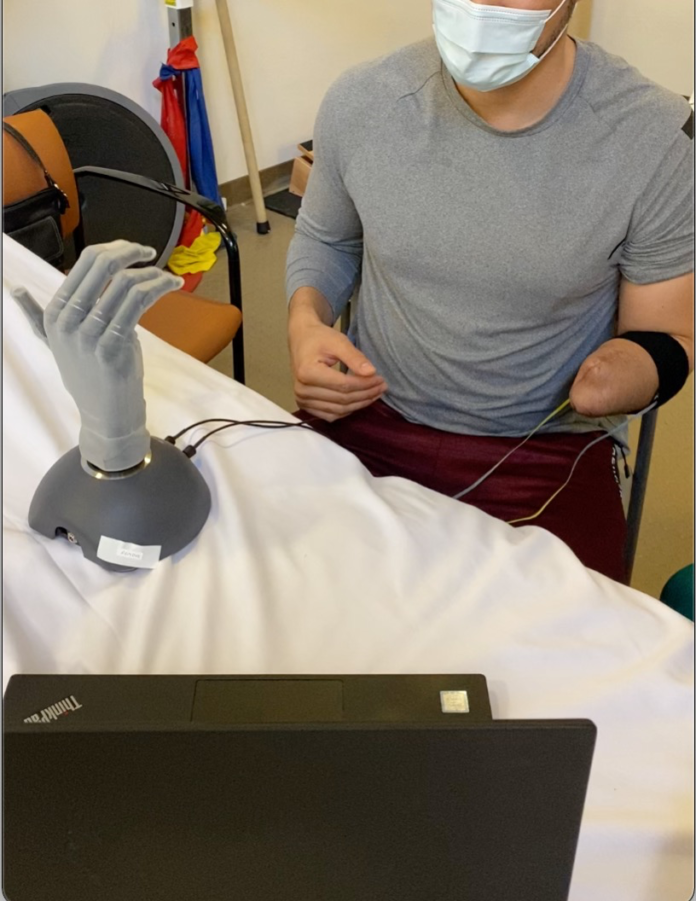
“We’re measuring movements using what we call EMG, or electromyography, and what we do is, we put a bunch of electrodes around the muscles that have been reinnervated surgically,” Schofield said. “And we can see that that measures the electrical activity of the muscles underneath the skin, and so anytime they think about doing a different hand movement, we can actually see different patterns of electrical activity.”
Using EMG has been the standard for smart devices worn by patients with amputations, but what Schofield and Joiner have been working on is a combination of EMG, ultrasound imaging and machine learning. Old prostheses movements used to require patients to contract their muscles in a specific pattern or a certain number of times, in order for the prosthetic limb to complete the patient’s intended movement. However, with Schofield and Joiner’s smart prosthetic device, these devices adapt to the patients, rather than forcing the patients to do the learning and adapting.
“What we do is, we put a small ultrasound transducer, like an ultrasound probe, on top of the reinnervation area, and what we can see is we can actually literally see the muscles underneath the skin moving in unique patterns depending on what the patient intends to do with their prosthetic limb,” Schofield said. “Using machine learning algorithms, the smart prosthetic device can actually pick out those patterns and predict what the users are trying to do.”
Schofield described the importance of tackling clinical progress of patients from a multidisciplinary approach as he looks to the hopeful advancement of prosthetic technology.
“As we look forward into the future, I think we’re going to continue to see technology advance, being more reliable in reading user intentions with more unique ways to communicate with the remaining neural anatomy after amputation,” Schofield said. “But even if we have the most advanced system that’s able to communicate perfectly with the user, if it’s not comfortable [for the patient], it’s not practical. So I see us having to apply these interdisciplinary, multi-disciplinary approaches in the future in which we’re working with prosthetists, we’re working with clinicians and we’re working with the patients as a collaborative team.”
Written by: Brandon Nguyen — science@theaggie.org