TFO device measures a fetus’s oxygen saturation levels non-invasively
By MONICA MANMADKAR — science@theaggie.org
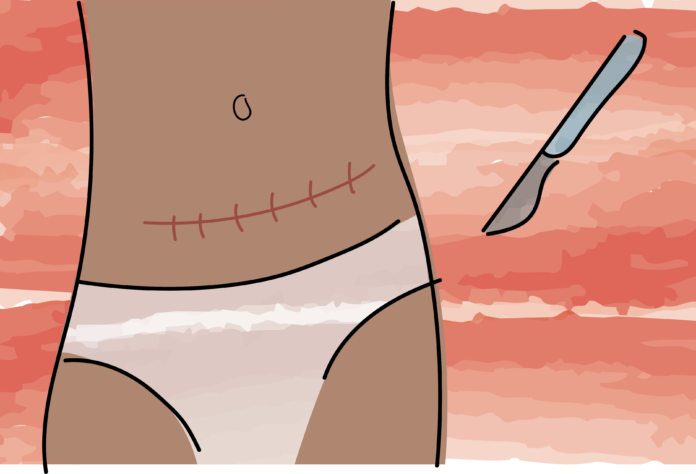
According to data published in Clinical Obstetrics and Gynecology in 2016, 60% of cesarean sections (C-sections) that are conducted due to potential hypoxia are unnecessary. Fetal hypoxia is a condition where the fetus is not delivered enough oxygen to continue growing.
Researchers at professor Soheli Ghaisi’s laboratory in the computer science and electrical engineering department have built a device to detect hypoxia in fetuses which can help decrease the number of unnecessary C-sections. The device measures the babies’ blood oxygen content through a non-invasive method.
“The birth of his youngest daughter started the idea for this device and research,” said Begum Kasap, a Ph.D. student working on this project at the Ghaisi lab.
The transabdominal fetal pulse oximeter (TFO) is used similarly to ultrasound transducers and generates a graphical user interface to calculate the oxygen saturation content, Kasap explained. Researchers are currently testing the efficacy of this device in pregnant female sheep.
“There is always a need to test the device in-vitro to evaluate the function of the device in large-animal studies,” said Dr. Aijun Wang, a professor in the department of biomedical engineering. “This is one of the reasons that testing with ewes was a better model since there is as large of a physiological difference.”
In order to calibrate the oxygen saturation system, the researchers draw blood from the anesthetized ewes’ fetuses to compare the TFO’s oxygen data to the actual oxygen saturation. This research and procedure strictly follow all mandates approved by the UC Davis Institutional Animal Care and Use Committee.
“Within the 13 studies that we’ve done since 2019, we were able to calculate the oxygen saturation with about a 10% mean absolute error,” Kasap said.
Testing of the TFO is extremely important for not only the improvement of the device but also for its integration into hospitals. The device has been tested on a small sample of healthy near-term pregnant patients. Although the researchers achieved 6.3 beats per minute (bpm) mean absolute error, they would want to have less than five bpm mean absolute error before sending the device for clinical application, Kasap said.
Looking at the future, Wang detailed how the research group hopes to get U.S. Food and Drug Administration approval for the device and improve it overall. For example, they would want to account for differences in skin color to serve a larger demographic.
To do so, Ghaisi, Kasap, Wang and the other researchers will continue conducting testing in both animals and humans to gather more data for the device’s overall improvement.
Written by: Monica Manmadkar — science@theaggie.org