Broad distribution of viable vaccine could take up to a year
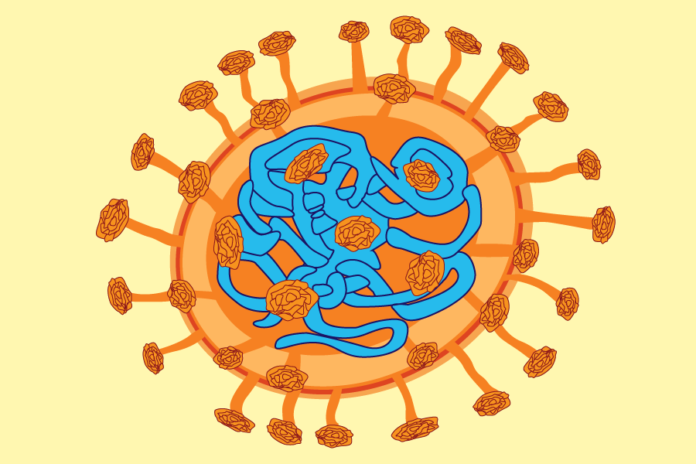
As the lives of people around the world have drastically changed due to the novel coronavirus, or COVID-19, pandemic, researchers from UC Davis have been working tirelessly to understand the mechanisms of the severe acute respiratory syndrome, coronavirus 2 (SARS-CoV-2), the virus which causes the COVID-19 disease, in order to develop a potential vaccine.
“Vaccines are based upon harnessing the ability of the immune system to recognize pathogens that they have counteracted before,” said Angela Haczku, a professor of medicine and associate dean for research at the UC Davis Medical School. “This feature or characteristic of the immune system is utilized when a small amount of the properties of the pathogen is being injected into the person.”
When an individual is exposed to a virus, a particle from the virus is recognized by a component of the immune system called a T lymphocyte, explained Haczku. Once T lymphocytes come into contact with these particles, they become memory T cells, which allow the immune system to recognize the virus if exposed to it again. Memory T cells allow helper lymphocytes to trigger B lymphocytes to produce the antibodies necessary to eliminate the viral particles.
The amount of time these memory T cells can live on in a person’s body depends on the nature of the antigen, otherwise known as a foreign substance or toxin. When vaccines are administered, with a specific antigen, one no longer has to worry about contracting a certain disease in the future as memory T cells remember how to fight it off. But certain viruses, such as influenza, are able to mutate and become infectious again, so new vaccines must be created in response. The ability to develop a vaccine for COVID-19 depends on the nature of the virus and whether researchers will be able to find a proper antigen that T lymphocytes will be able to remember as the virus ages.
“We don’t know what’s happening with [COVID-19] because humankind never encountered a coronavirus pandemic before,” Haczku said. “This is the very first time and therefore we never had the need to develop vaccines against coronavirus.”
Although COVID-19 is novel, as the virus which causes it is not the same as the viruses that cause other coronaviruses, previous research already conducted on other coronaviruses has contributed to some of the early progress for UC Davis researchers, according to Denis Hartigan-O’Connor, an associate professor in the department of medical microbiology and immunology and a core scientist at the California National Primate Research Center (CNPRC).
“We learned from [previous research] about basically how to grow this virus, what things might inhibit it, what are some vaccine strategies that could be tried and then we start to think about the biology of this new agent and whether these strategies are applicable,” Hartigan-O’Connor said.
Hartigan-O’Connor is a part of a group of researchers at the CNPRC working toward developing the first animal model in learning how SARS-CoV-2 affects monkeys. Smita S. Iyer, an assistant professor and core scientist at the infectious disease unit at the CNPRC, explained that once an animal model is developed, researchers will be able to answer fundamental questions that are difficult to answer with a human model. For example, factors like the mode of infection and viral concentration in the body, both of which are difficult to control for in humans, can be accounted for in these essential animal models.
“We are not going to win the race to make a vaccine in academia because of resources,” Iyer said. “We just cannot compete with biotech [companies] and pharmaceutical [companies]. But what we can do and what we do really well is to understand the immune mechanism of protection, and so if we use that kind of approach to design a vaccine, that might inform the field.”
Hartigan-O’Connor explained that his group plans to test a vaccine on monkeys in the next three to four months. Once they establish a candidate in which the vaccine seems to be effective, researchers will be able to quickly move onto human trials, Hartigan-O’Connor predicts. Iyer speculates that it will take another 12 months or, optimistically, closer to the end of the year for a viable COVID-19 vaccine for humans to be widely distributed .
“That seems like a long time to get to humans, but it’s actually quite a short time scale because it’s so important to make sure we get a vaccine that makes the situation better and not worse,” Hartigan-O’Connor said.
Despite the world’s uncertainty concerning this virus, there have been promising results. A recently published study illustrates how monkeys that have been infected by the COVID-19 virus once are protected from reinfection. Although this is just one study, this information allows researchers to be hopeful that infected and recovered patients are protected from reinfection and that a vaccine will prove to be helpful in this pandemic, according to Iyer. This also raises the possibility of herd immunity, when there are enough individuals who are protected from the virus so that it is unable to find new hosts, slowing transmission.
Although her lab did not initially have any particular expertise in coronaviruses, Iyer explained that her ability to study SARS-CoV-2 is due to a team effort of her graduate students Sonny Elizaldi and JW. Roh, colleagues Chris Miller and Koen Van Rompay and many other essential faculty members from the Center for Immunology and Infectious Diseases (CIID) and CNPRC.
Haczku described the nature of this virus as “sneaky” since it did not cause its original host, most likely a bat, to become sick but was still able to attack the immune systems of different species. This means everyone must practice proper hygiene and social distancing, as asymptomatic people may also be spreading the virus.
“We have to fight against this very ruthless and sneaky virus. It’s kind of a combat situation,” Haczku said. “In order to win this fight, we all have to unite, even people who don’t know anything about vaccination or how the viruses work. It would be nice if we understood the importance of fighting against it together.”
Written by: Michelle Wong — science@theaggie.org