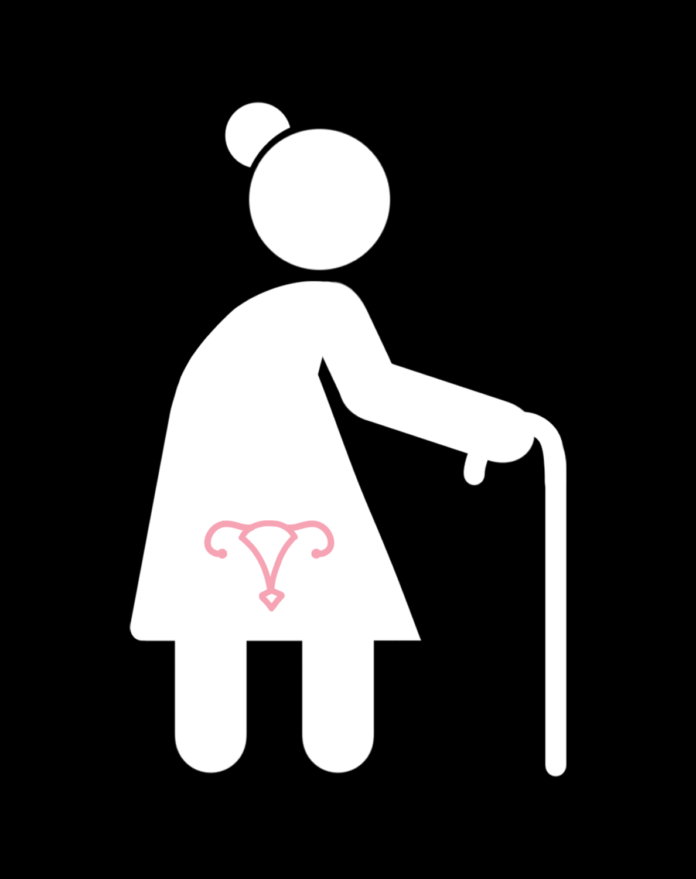
Current screening guidelines do not sufficiently assess this demographic for cervical cancer
By LILLY ACKERMAN — science@theaggie.org
A recent study by researchers at UC Davis Health’s Comprehensive Cancer Center found that nearly one in five new cervical cancer diagnoses in California are in patients over the age of 65 and that these cases are usually late-stage and have low survival outcomes.
According to Julianne Cooley, the lead author of the study and a senior statistician at UC Davis Health, this finding is contrary to current guidelines for cervical cancer screenings in patients who are 65 years of age and older.
“Current guidelines recommend not screening women [over] 65 years [old] with history of normal Pap [Pap smear] and/or HPV [Human Papillomavirus] tests,” Cooley said via email. “However, we found that nearly 1 in 5 new cervical cancer diagnoses are among women [older than] 65. Furthermore, women in this age group are usually diagnosed late stage (71%) and have very poor survival compared to other age groups.”
These higher-risk cases found in the study suggest that guidelines are missing a demographic that still needs to be screened, especially since consistent screening can catch an early-stage disease, which has a much higher survival rate than late-stage disease.
Patients over the age of 65 might consider resuming regular screenings to mitigate the risks identified by the study.
“Screening can prevent or detect cervical cancer at stage I, when the chance of survival is excellent,” Cooley said. “So, women of any age who are not up-to-date on cervical cancer screenings should schedule a screening and make sure to follow up on any abnormal results.”
Prior studies have shown that many patients of all ages are not up to date with screenings in the first place, so the reason for an increase in late-stage disease in patients over the age of 65 might be due to the lack of consistent screening even before they reach this age, according to Cooley.
It is therefore critical that patients in this age range are evaluated for prior screening history, and any abnormal results are followed up with more care.
“There remains a significant burden of advanced cervical cancer in women [older than] 65,” the study reads. “Efforts should be made to better understand how the current screening paradigm is failing women of 65 years and older. Future work should focus on determining past screening history, lapses in follow-up care, and non-invasive testing approaches.”
The authors hope to emphasize the importance of regular screening leading up to the 65-year mark, as well as to encourage those older to be tested again, especially if they were behind on screenings before they reached this age. In doing so, they hope to lessen the alarming number of late-stage diagnoses in this demographic.
“I hope that as a result of our findings, more women approaching 65 will get screened regularly and that any women who were not up to date on their screenings prior to turning 65 will receive a catch-up test to prevent unnecessary cervical cancer deaths,” Cooley said.
Written by: Lilly Ackerman — science@theaggie.org